Twin-Twin Transfusion Syndrome
I want to start sharing a bit more educationally-focused information here. However, in line with my long history of utilizing social media to connect with patients and understand the human side of the story, I hope to employ my non-medical, digital-friends to inspire these topics.

Hannah from Daytrips & Diapers has graciously given me permission to discuss/link her in this post. She is pregnant with monochorionic – diamniotic twins and was diagnosed with twin-twin transfusion syndrome (TTTS) at 16 weeks. She recently traveled to the nearest fetal surgery center, >8 hours from her home, and underwent a procedure aimed at decreasing placental connections and improving blood flow (and hopefully, outcomes) for both babies.
She then experienced a known complication of the surgery, however at the time of my writing is still joyfully pregnant with both of her twins. Hop over to her blog or Instagram and follow her story for the human side of medicine. Read on below if you’re interested in the medical side – I’ll discuss diagnosis, pathophysiology, and treatment of TTTS below.
What is Twin-Twin-Transfusion Syndrome?
- A complication isolated to monochorionic (one placenta) twin pregnancies where vascular connections on the shared placenta develop pressure/flow gradients. This allows one twin (“donor”) to become anemic and the other (“recipient”) to become plethoric and begins a cascade of physiologic changes which can become catastrophic.
How Often Does This Occur?
- The incidence in mo/di pregnancies is about 10-15% and bout 6% in mo/mo twins develop TTTS. Dichorionic twins cannot develop twin-twin transfusion syndrome, as they have two placentas.
How Is Twin Twin Transfusion Syndrome Diagnosed?
- The diagnosis is made clinically by ultrasound. It is classically identified by “Poly-Oli Sequence”
-
!! This will be how it’s presented on USMLE-type exams. !!
- Refers to polyhydramnios of recipient twin and oligohydramnios of donor twin.
- Occasionally, there will be such severe oligo in the donor twin that it develops “Stuck Twin,” which is essentially the ultrasound appearance of a donor twin being stuck to the placenta. Anatomically, this results from such severe oligohydramnios that the amniotic sac is lying directly against the fetus.
-
!! This will be how it’s presented on USMLE-type exams. !!
What’s The Pathophysiology?
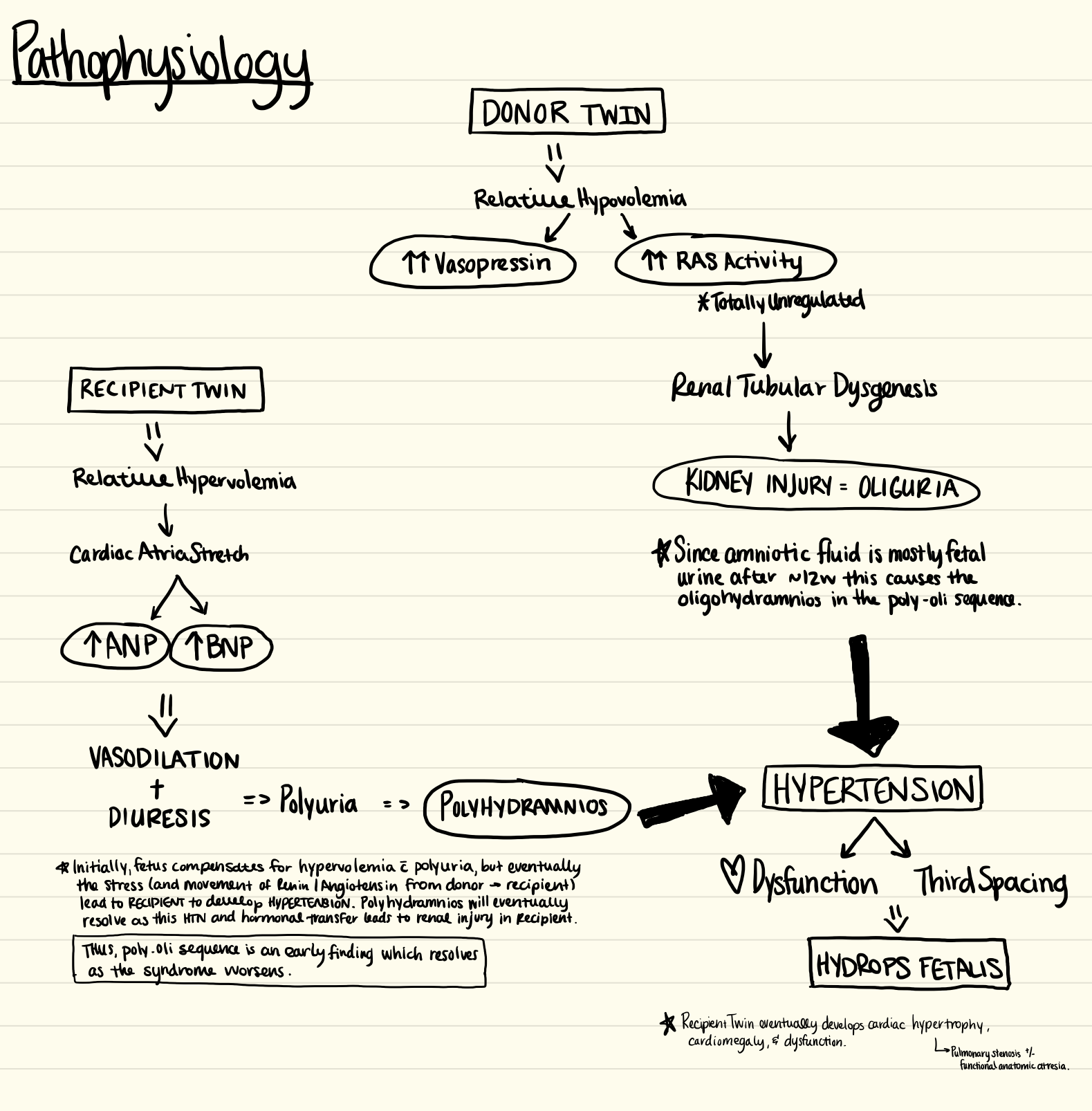
- DONOR: Relative Hypovolemia –> Kidney Injury –> Hypertension
- RECIPIENT: Relative Hypervolemia –> Vasodilation/Diuresis –> Polyhydramnios –> Hypertension
- BOTH: Hypertension –> Cardiac Dysfunction –> Hydrops Fetalis
- Click Flow Chart to enlarge for more detail
How Bad Is It?
- It depends on the stage.
- Quintero Staging
- I: Poly-Oli Sequence (Visible Donor Bladder + Normal Doppler Flow)
- II: Poly-Oli Sequence + Collapsed Donor Bladder (Normal Doppler Flow)
- III: Poly-Oli Sequence + Non-Visualized Bladder + Abnormal Doppler Flow
- IV: Hydrops Fetalis in one or both twins
- V: Fetal Death in One or Both Twins
How Is It Treated?
- The treatment course depends on gestational age at diagnosis and severity/stage, however there are basically 3 options:
- Expectant Management (i.e. No intervention, just watch)
- Fetoscopic Laser Ablation
- Amnioreduction (removing the “Poly” of the poly-oli sequence)
What is Fetoscopic Laser Ablation?
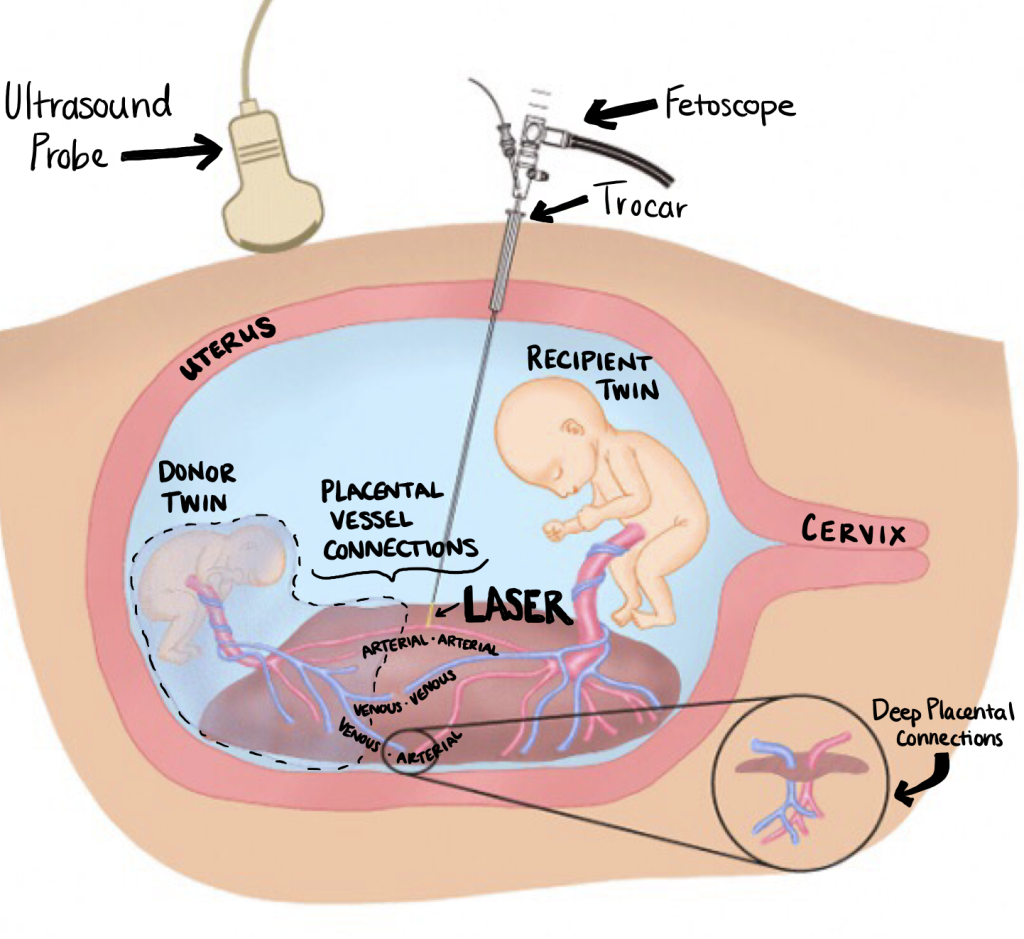
- This is a surgical procedure which is performed by fetal surgeons. It involved laser cauterization of superficial anastomotic placental connections through minimally invasive fetoscopes.
- Maternal preparation includes complete ob ultrasound (including placental location, distance between umbilical cord insertions, and fetal locations/presentation/sizes) and medications (antibiotic + tocolytic +/- steroid for fetal lung maturity depending on gestational age). The procedure is enerally performed with local or regional anesthesia + sedation
Fetoscopic Laser Ablation Procedure Steps
- Skin incision with scalpel (site determined by placental and fetal locations)
- Entry Options
- 18g hollow-needle introduced through maternal abdominal wall and placenta
- J-Wire guide placed –> Needle removed –> Catheter placed over guidewire with US guidance
- Metal trocar placed through cannula to allow for uterine entry
- 2-3mm Fetoscope (with or without angled scope, depending on entry-technique and surgeon preference) inserted
- 18g hollow-needle introduced through maternal abdominal wall and placenta
- Identify all fetal extremities to avoid injury
- Identify vascular equator
- Typically in recipient amniotic sac (parallel to “stuck twin” if present)
- Anastomoses are mapped out and typed
- Types include arterial-venous (AV), venous-arterial (VA), arterial-arterial (AA), and venous-venous (VV)
- Visible connections are coagulated using laser ablation
- Sequential selective ablation (AV –> VA –> AA –> VV) reduces intrauterine fetal death rates
- Vascular equator re-identified and coagulated
What are the Complications and Outcome?
- Complications of the Procedure
- Preterm Labor
- Preterm Delivery (Avg. gestational age is 31-33w)
- Preterm Premature Rupture of Membranes (PPROM)
- Intertwin Membrane Rupture
- Essentially bringing all the risks of monoamniotic twins into play (like cord-entanglement)
- Pseudo-Amniotic Band Syndrome
- Fetal Demise
- Perinatal Survival Rates: 65%
- Still with long-term neurodevelopmental, cardiac, & renal morbidities associated with survival.
- OVERALL AFTER LASER
- 50% both survive
- 33% one survivor/one fetal demise
- 33% both with fetal demise
- Perinatal Survival Rates: 65%
Wow, Those Odds Look Bad…
- They are daunting, for sure. However, TTTS severe enough to warrant laser-intervention which is left completely un-treated will result in fetal death of one twin in nearly 100% cases and both twins in >90%. These outcomes, when appropriate candidates are selected, are far superior to no treatment.
That’s a brief overview of TTTS and fetoscopic laser ablation. I’ve done a few LIVE Q&As on Twins, I’ll try to round those up to get on YouTube for a more thorough discussion of the pathophysiology and also the different types of twins.
It’s so important when learning about things like this that we don’t forget there’s a human (or, in this case 3) on the other side of our text books. Hop over to the blog and/or IG linked in the intro paragraph for a view into how this looks from a patient perspective.
